Introduction
Anterior resection is one of the most commonly performed surgeries for diseases affecting the rectum and lower sigmoid colon. Surgeons often recommend this procedure for conditions such as rectal cancer, diverticular disease, benign tumors, strictures, and severe inflammatory bowel disease.
Because it is considered a major abdominal operation, patients and medical students frequently search for reliable and clear information about anterior resection surgical steps. This comprehensive guide offers a detailed explanation of each step, ensuring accurate understanding while maintaining strong SEO.
If you are researching this procedure, preparing academic material, or creating medical content, this article will provide everything you need to know about the surgical steps of anterior resection, its purpose, preparation, technique, and postoperative expectations.
What Is Anterior Resection?
Anterior resection is a surgical procedure performed to remove the diseased portion of the rectum or sigmoid colon while preserving the anal sphincter. This allows patients to avoid a permanent colostomy in most cases.
The main goals of anterior resection include:
- Removing tumors or diseased tissue
- Preserving normal bowel function
- Preventing cancer spread
- Restoring continuity of the gastrointestinal tract
The surgery can be performed using open surgery, laparoscopy, or robotic-assisted techniques, depending on the patient’s condition and the surgeon’s expertise.
Indications for Anterior Resection
Surgeons typically recommend anterior resection for:
- Rectal cancer (mid or upper rectum)
- Sigmoid colon cancer
- Chronic diverticulitis
- Precancerous polyps
- Ischemic colitis
- Large benign tumors
- Rectal strictures
- Inflammatory bowel disease complications
The choice of technique depends on tumor location, staging, patient health, and anatomical considerations.
Pre-Operative Preparation
Before performing anterior resection, the surgical team follows a structured preparation plan to ensure the best outcome.
Diagnostic Evaluation
- Colonoscopy
- CT scan or MRI
- Blood tests
- Tumor markers (CEA for colorectal cancer)
Bowel Preparation
Surgeons may recommend:
- Full bowel cleansing with oral laxatives
- Low-residue diet
- Antibiotic prophylaxis
Anesthesia Assessment
A pre-operative anesthesia evaluation ensures the patient is fit for general anesthesia.
Informed Consent
The surgical team explains:
- Risks
- Benefits
- Possible complications
- Potential need for a temporary stoma
Anterior Resection Surgical Steps (Detailed Explanation)
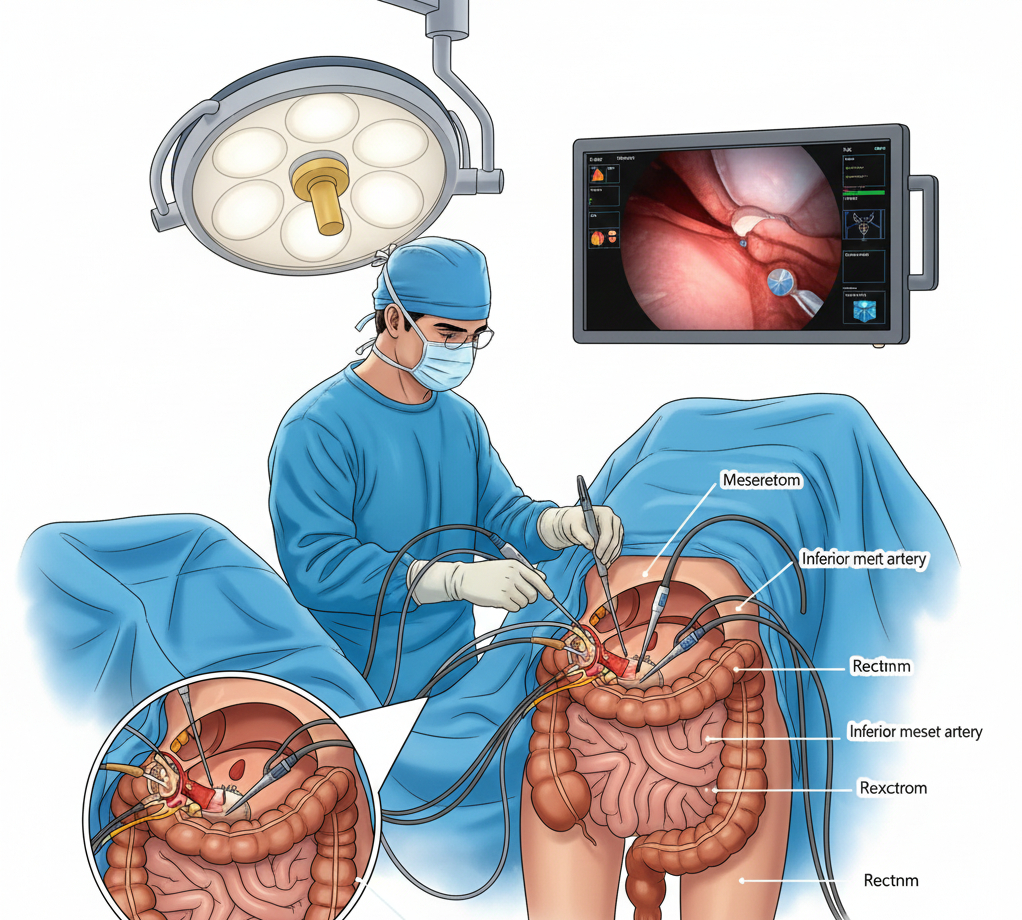
Below is a detailed, medically accurate outline of the anterior resection surgical steps, covering both open and laparoscopic approaches.
Patient Positioning and Anesthesia
The surgery begins with:
- Administration of general anesthesia
- Patient placed in lithotomy or modified Lloyd-Davies position
- Arms secured to prevent pressure injuries
- Abdomen cleaned and draped in sterile fashion
This position improves access to the pelvis and lower abdomen.
Abdominal Entry
Depending on technique:
Open Surgery:
- A midline incision from umbilicus to pubis
- Careful entry into the peritoneal cavity
Laparoscopic Surgery:
- Trocar insertion
- CO₂ insufflation to create a pneumoperitoneum
- Placement of 4–5 ports for instruments
Exploration and Assessment
The surgeon inspects:
- Tumor location
- Lymph nodes
- Liver and peritoneum
- Surrounding organs
The goal is to ensure operability and rule out metastasis.
Mobilization of the Sigmoid Colon
The surgeon performs:
Medial-to-lateral dissection
- Identification of the inferior mesenteric artery (IMA)
- Ligation and division of IMA and IMA vein (if oncologically required)
- Development of avascular planes
Lateral mobilization
- Opening the white line of Toldt
- Freeing the sigmoid colon from the retroperitoneum
This step creates space for bowel removal and anastomosis.
Mobilization of the Rectum
The rectum is carefully mobilized using:
Total Mesorectal Excision (TME)
- Standard for rectal cancer
- Sharp dissection along the mesorectal fascia
- Preservation of autonomic nerves
Partial Mesorectal Excision (PME)
- Used for upper rectal lesions
- Less extensive than TME
Identification and Protection of Key Structures
The surgeon protects:
- Hypogastric nerves
- Ureters
- Iliac vessels
- Pelvic nerves
Preserving these prevents urinary and sexual dysfunction.
Resection of the Diseased Segment
After mobilization:
- The proximal colon is divided using a surgical stapler
- The rectum is divided below the tumor margin
- Adequate oncologic margins are ensured (usually 2–5 cm depending on tumor type)
The diseased section is removed completely.
Creation of the Anastomosis
To restore bowel continuity, the surgeon connects the proximal colon to the remaining rectum.
Types of Anastomosis:
Stapled Anastomosis
The most common technique:
- Circular stapler inserted transanally
- Proximal colon attached to anvil
- Stapler fired to create a secure colorectal connection
. Hand-Sewn Anastomosis
Less common but useful in complex anatomy.
Air Leak Test
The surgeon performs a leak test by:
- Filling the pelvis with saline
- Insufflating air through the anus
- Checking for bubbles (indicating leakage)
If a leak is detected, additional sutures or reinforcement is applied.
Formation of a Temporary Stoma (If Needed)
In high-risk cases, a temporary ileostomy may be created to:
- Protect the anastomosis
- Reduce leak risk
This stoma is usually reversed after healing.
Closure and Completion
Finally:
- Surgical area irrigated
- Hemostasis confirmed
- Incisions closed layer by layer
- In laparoscopic cases, trocars are removed and port sites closed
The patient is awakened from anesthesia and transferred to recovery.
Post-Operative Care After Anterior Resection
Recovery involves:
Monitoring
- Heart rate
- Blood pressure
- Urine output
- Pain control
Diet Advancement
- Clear liquids
- Soft foods
- Normal diet as tolerated
Early Mobilization
Walking helps prevent:
- Blood clots
- Pneumonia
- Constipation
Follow-Up
Patients must attend post-operative checkups to monitor:
- Healing
- Bowel function
- Oncology treatment plan (if cancer-related)
Possible Complications of Anterior Resection
Common potential complications include:
- Anastomotic leak
- Infection
- Bleeding
- Deep vein thrombosis
- Ileus (temporary bowel paralysis)
- Urinary or sexual dysfunction
- Stoma-related issues
Thanks to modern techniques, complication rates continue to decrease.
Benefits of Anterior Resection
Patients benefit from:
- Organ preservation
- Avoiding permanent colostomy (in most cases)
- Reduced cancer recurrence
- Better quality of life
- Faster recovery with laparoscopic or robotic surgery
Conclusion
Understanding the anterior resection surgical steps helps patients, students, and healthcare professionals gain clarity about this life-saving procedure. From pre-operative preparation to rectal mobilization, resection, and anastomosis, each step requires precision, expertise, and knowledge of pelvic anatomy.
Whether performed for cancer or benign disease, anterior resection remains one of the most effective surgical treatments for rectal and sigmoid pathology. With advancements in minimally invasive techniques, patient outcomes continue to improve year after year.